Case # 1. A 55 year old white male who p/w a 2 month h/o headache, progressive mental status deterioration, persistent pleocytosis and evidence of leptomeningeal enhancement on MRI secondary to tuberculous meningitis.
Taken from: http://www.bioquellus.com/interface/assets/images/content/Mycobacterium_tuberculosis_14313982_1.jpg
1. The case was diagnosed late in the course of the disease as all infectious disease work-up had been unremarkable. A prior brain and meningeal biopsy were also non-revealing. The diagnosis was only made when a second meningeal and brain biopsy revealed sparse evidence of AFB associated with granulomatous changes. Despite initiation of anti-TB treatment, he expired.
2. The case illustrates how hard it is to suspect and diagnose tuberculosis among persons living in low endemic areas. CNS tuberculosis carries a high mortality rate. Delay in treatment (even for a few days) is associated with mortality. If a high index of suspicion exists, treatment should be initiated while waiting for work-up.
3. To increase the sensitivity of CSF AFB analysis, a minimum of 3 serial lumbar punctures should be performed. This has been reported to increase CSF AFB sensitivity from 37 to 87% (read here).
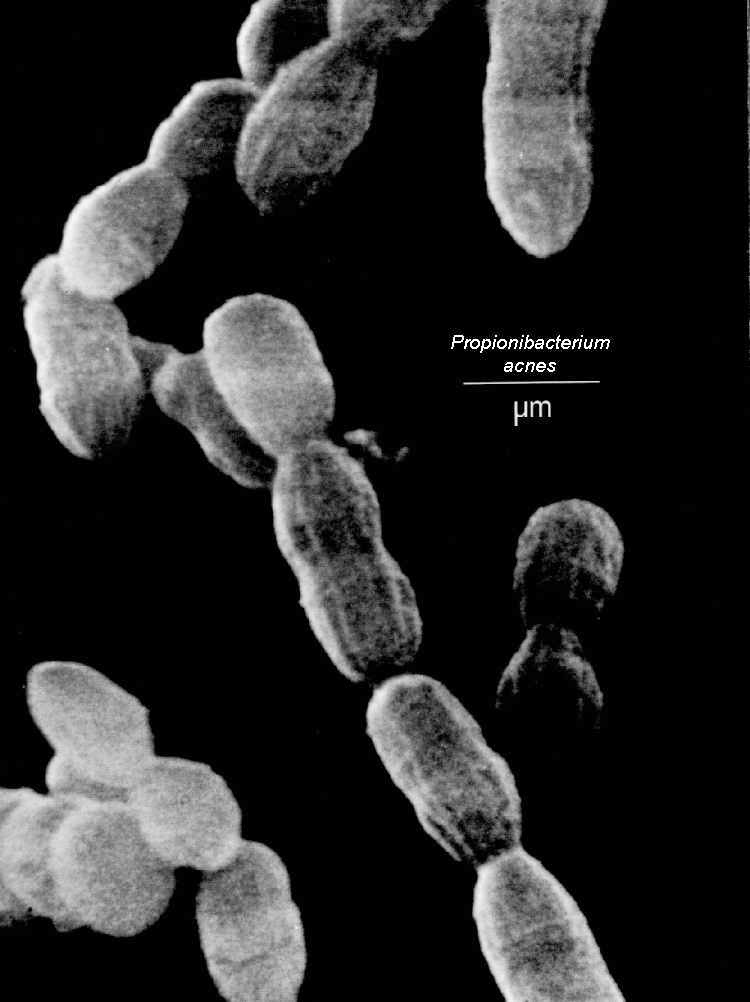
4. This case also highlights the potential use of next-generation sequencing to detect occult infection as illustrated by our Propionebacterium acne chronic meningitis case from Oct 14, 2014 and by the NEJM case of neuroleptospirosis as previously referenced.
5. Treatment of CNS tuberculosis (and pericarditis), in most cases, requires use of adjunctive corticosteroids to prevent immune reconstitution syndrome (so called 'paradoxical reaction') which can be life-threatening.
Case # 2. A 2 month old infant p/w fever, respiratory failure, hepatosplenomegaly, bilateral hydronephrosis, urinary infection from Serratia, and pneumonia from Burkholderia secondary to chronic granulomatous disease (CGD).
Taken from: http://www.immunopaedia.org.za/fileadmin/gallery/Chronic%20Granulomatous%20Disease/chronicgranulomatousdisease1.jpg
1. CGD is caused by a genetic defect that prevents generation of supreroxide radicals that fight infection.
2. Remember that the autosomal recessive variant of CGD can occur later in life (as adolescents or adults).
3. Suspect CGD in an apparently healthy patient with recurrent or severe infection with Serratia, Burkholderia, Nocardia, Aspergillus, Salmonella, and Bacillus Calmette-Guerin (BCG).
4. One peculiar feature of CGD is the formation of granulomas that lead to visceral obstruction (e.g. small bowel obstruction, hydroureter, hydronephrosis).
5. CGD can be associated with the occurrence of hemophagocytic lymphohistiocytosis (HLH) and autoimmune conditions. CGD can mimic systemic lupus erythematosus (SLE) and inflammatory bowel disease.
6. The use of Bactrim, itraconazole, and interferon gamma is the cornerstone of prophylaxis against infections among persons with CGD.