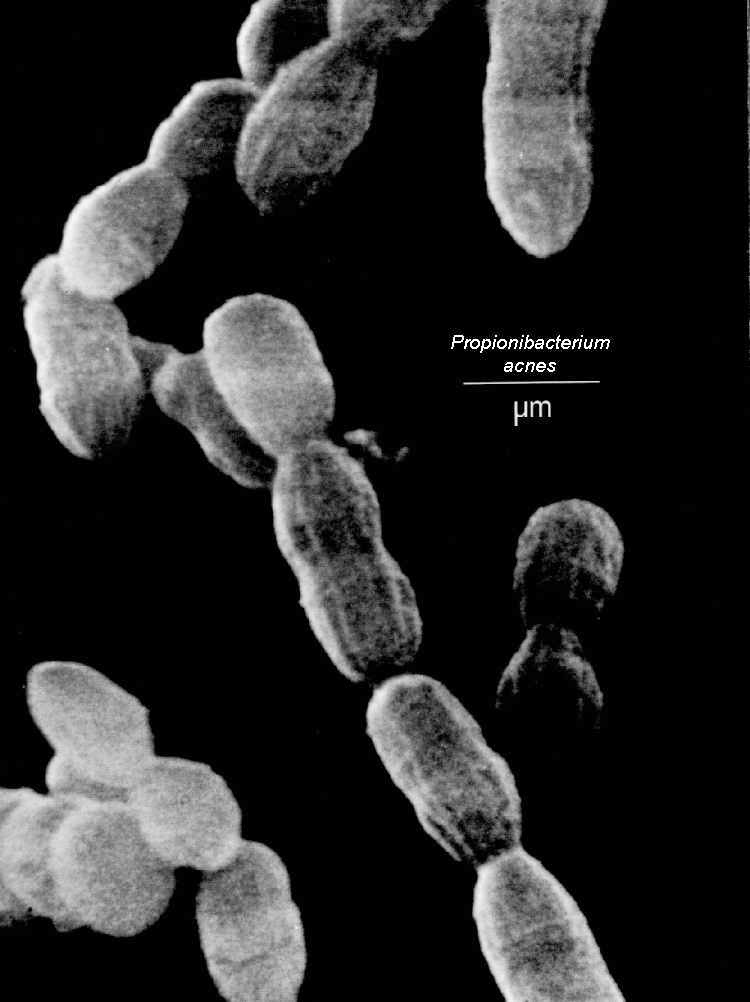
Case 1. A 43/M with CML s/p stem cell transplantation 2 years ago who p/w a 1.5 year h/o chronic lymphocytic meningitis associated with obstructive hydrocephalus secondary to chronic CNS Propionebacterium acne infection
Taken from: http://luskiewnik.strefa.pl/acne/propionibacterium_acnes_files/propioni.jpeg
1. Propionebacterium acne has been shown in case reports and case series to cause chronic meningitis even in patients with no history of neurosurgical procedure (read here). It is seen in both immunocompromised and immunocompetent individuals. In most cases, a mononuclear-predominant pleocytosis is appreciated from the CSF.
2. Another learning point is that, the diagnosis of Propionebacterium acne chronic meningitis in this case was aided by the use of next generation sequencing (which maybe more sensitive that 16S rRNA gene sequencing). Read here regarding the NEJM article that chronicles how a patient with chronic neuroleptospirosis was diagnosed by this method.
Case 2. A 15-month old child with cartilage-hair hypoplasia syndrome (associated with severe combined immunodeficiency) presents with persistent diarrhea secondary to Norovirus infection
Taken from: http://upload.wikimedia.org/wikipedia/commons/a/ae/Norovirus_4.jpg
1. Norovirus infection is self-limited and typically lasts for 2-3 days. However, in immunocompromised patients, the diarrhea can persist for several weeks to months and is sometimes associated with substantial symptoms that include severe debilitation and weight loss. It should be added in the differential diagnoses of immunocompromised patients with chronic diarrhea that eludes diagnosis. Further readings here and here.
2. Norovirus is diagnosed with stool PCR. There is no specific treatment for infection apart from supportive care. In immunocompromised patients, reduction of immunosuppression may help. Good evidence with the use of enteral immunoglobulins, nitazoxanide, and ribavirin is lacking at present.
Case 3. A 68/F with cochlear implants presents with Streptococcus pneumoniae meningitis, pneumonia, and endocarditis (the Austrian triad/syndrome)
1. One needs to rule out endocarditis with a TEE in a patient with co-occurrence of pneumococcal meningitis and pneumonia. At least 2/3 of patients with pneumococcal endocarditis have concurrent pneumococcal pneumonia and meningitis.
2. Patients who develop acute otitis media after cochlear implantation have the greatest risk of subsequent pneumococcal meningitis. Most common organisms isolated are Streptococcus pneumoniae, Haemophilus influenzae, Streptococcus pyogenes, Branhamella catarrhalis, Staphylococcus aureus, mixed organisms, and gram negative bacilli.
3. Patients with cochlear implants and immunocompromising conditions (and recently, patients at least 65 years, read here) should get 13-valent pneumococcal conjugate vaccine on top of 23-valent pneumococcal polysaccharide vaccine.

No comments:
Post a Comment